The Fraser Eye Care Center Doctors have either authored or reviewed and approved this content.
A Retinal detachment is when the retina, in the back of the eye, separates from its underlying supportive tissue. The retina cannot function when these layers are detached, as such if not reattached quickly, permanent vision loss may result.
This is generally a result of a gel-like material that fills the back of the eye (called vitreous humor). As we age vitreous shrinks and becomes more liquid with aging, causing it to slosh around. And because the vitreous is attached to the retina with tiny strands of cells, it pulls on the retina as it shrinks. Sometimes it separates the retina from its underlying supportive tissue.
Symptoms of having a retinal detachment include the onset of new floaters, flashing lights, a “curtain” or area of darkness that may encroach on your vision. There is no pain associated with having a retinal detachment.
Retinal detachments occur at a frequency of 1 for every 10,000 people. It is most common in people who are in their 50s and 60s with a higher frequency in males than females. Risk factors to having a retinal detachment include:
The long term outcomes depend on the duration of the detachment and whether the macula was detached. If the detachment is limited or simply a retinal tear, laser or cryotherapy (freezing) is generally performed. For some detachments a procedure called pneumatic retinopexy is performed where air or gas is injected into the eye in conjunction with laser or cryotherapy. Doctors provide patients with specific head position instructions which allow the bubble to float up against the compromised retina and keep it in position as it heals.
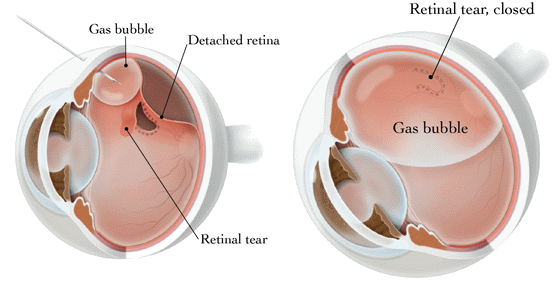
In other cases of retinal detachment, vitrectomy or vitrectomy with scleral buckle is performed. Vitrectomy is a technique where the vitreous gel and any scar tissue in the eye is removed, after the retina is reattached, a gas bubble is filled help hold the retina in position. The bubble generally lasts in the eye for several weeks and is gradually absorbed by the body. A silicone oil bubble can also be used, but is generally reserved for more complex cases. To maintain the gas or silicone tamponade, you must lie face down, sometimes for as long as two weeks!
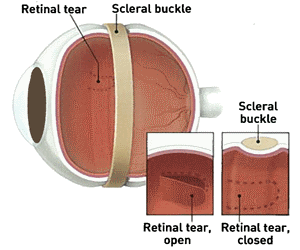
Vitrectomy with Scleral Buckle involves attaching a small band of silicone or plastic to the outside of the eye (sclera). This band compresses (buckles) the eye inward, reducing the pulling (traction) of the retina and thereby allowing the retina to reattach to the interior wall of the eye.
The most common complication to Vitrectomy surgery is Cataract development. Cataracts can occur rather quickly after a vitrectomy surgery, generally within the first year following surgery.
Other potential complications include:
It is important to remember these potential complications are less of a concern compared to not fixing the retinal detachment which will lead to permanent vision loss.
The Fraser Eye Care Center Doctors have either authored or reviewed and approved this content.